45 yr old male patient, church pastor by occupation,
came to the hospital with chief complaints of
Shortness of breath for 4 days 1 1/2 yr back
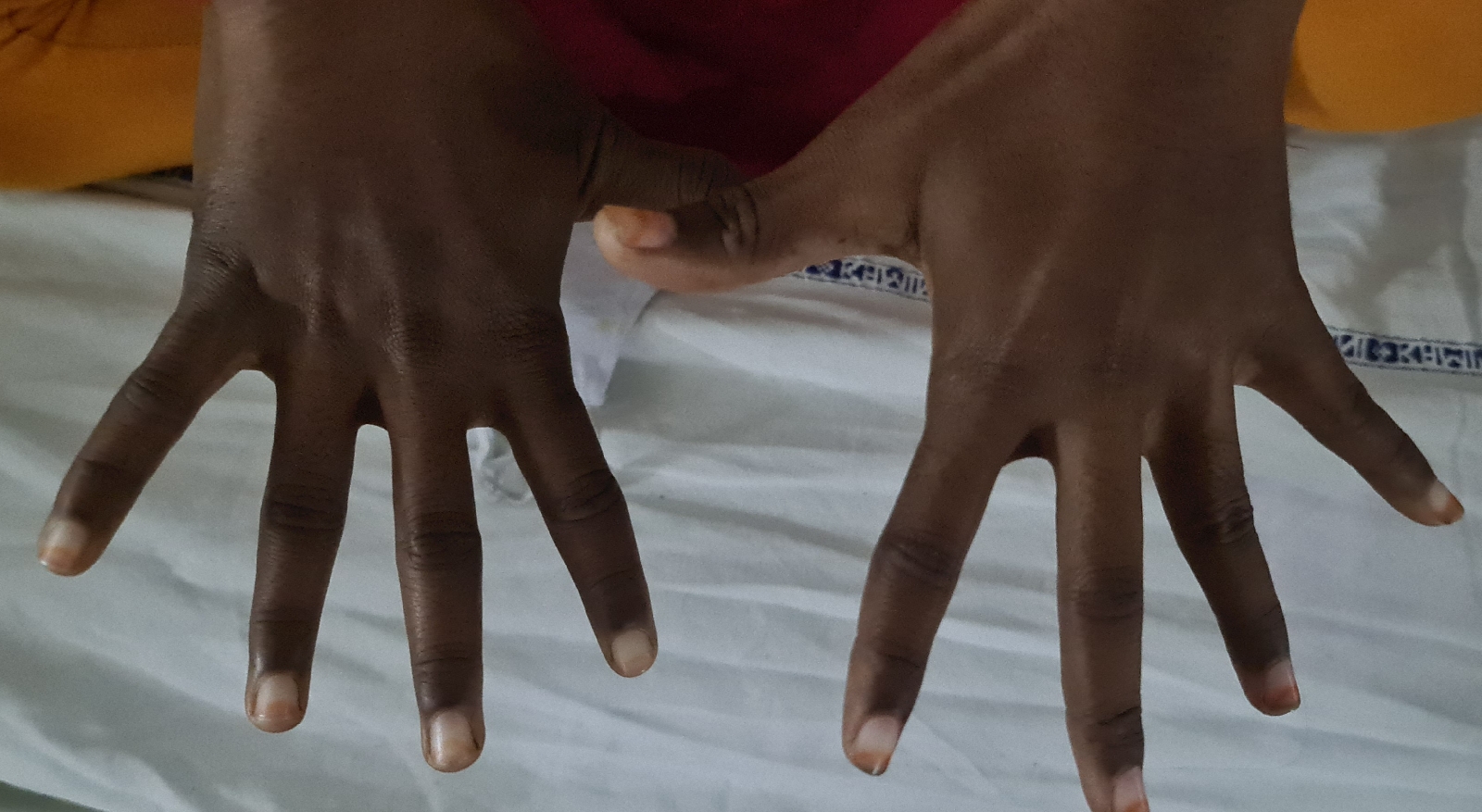
Pedal edema for 4 days 1 1/2 yr back
Decreased urine output for 4 days 1/1/2 yr back
The patient was apparently asymptomatic 15 months back when he developed vomitings, loss of appetite and decreased urine output for which he was taken to the hospital where he was diagnosed with CKD. Since then the patient has been undergoing about 4-5 sessions of dialysis every month.
Had h/of hearing loss since 8 months secondary to diuretics and initially used hearing aids but stopped using it due to one sided headache
Underwent catarct surgery left eye in July 2021 and right eye in Nov 2021
Patient presently on fern cath placed in month of May
K/c/o
CKD on MHD since 11/2 year
HTN since 10 years on tab nicardia 10 mg
DM since 10 years. Was on tab metformin but stopped using medication since starting dialysis sugars were under contolled
Yesterday during dialysis after 2 1/2 hrs of session patient complained of sob
On examination
Patient conscious
Pulse feeble
Bp-60/NR
Spo2 : 88 on RA
Temp- 100F
RR- 24 cpm
BP- 80/50 mmhg with NA 20 ml/hr
Spo2- 98% at 10 L of oxygen
GRBS- 101 mg/dl
R/S : Inspiratory creprts + on left IAA and ISA
CVS : S1 and S2 +
P/A : soft
CNS : NO FND
Pupils NS RL
Right upper lid edema + with congestion on operated right eye
Provisional Diagnosis: CKD on MHD with HTN with hearing loss with Shock secondary to infective endocarditis ( tricuspid valve) secondary to permcath
Rx:
Fluid restriction <1.5 lit/day
Salt restriction < 2 gm/day
Inj NA 2 amp in 48 ml NS @ 20 ml/hr ( increase or decrease to maintain map of 55 to 65 )
Tab. Nodosis 500 mg PO/BD
Tab. Shelcal CT PO/OD
Tab Orofer XT PO/OD
Tab BIO D3 0.25 mg PO/OD
Inj Erythropoietin 4000 IU SC/weekly once
https://drive.google.com/file/d/1KtaxUxW7QWiAB84YQyB1Y3tzEL_gt2Kq/view?usp=drivesdk
On 18/11/2021
At 12.30 am -pt complained of sudden onset sob with spo2:88% on room air, bp -170/100mmhg with inj norad -ds@6ml/hr, on auscultation diffuse end expiratory wheeze +, patient was given nebulisations and oxygenation, when he became unresponsive, with no central pulse, cpr was initiated and 12cycles were done, inspire of which patient could be resuscitated and was declared dead at 1.45 am